Board votes to modify opioid investigations program
Comments: 5 comments Print Friendly Version | Share this itemCurrently SOPI, which was implemented in April 2016, investigates NCMB licensees who have had multiple patient deaths due to opioid overdose AND licensees who write large numbers of high-dose opioid prescriptions (See “Current SOPI investigative criteria” below). The Board has proposed rule changes to amend the existing selection criteria. The Board is also contemplating new selection criteria to identify prescribers whose medical practices display characteristics associated with potentially inappropriate opioid prescribing.
NCMB welcomes feedback on the proposed rule changes. A public hearing is scheduled for May 1 at the Board’s Raleigh offices. Written comments may be submitted to rules@ncmedboard.org.
How does NCMB want to change the “patient deaths” criteria?
Currently, the Board opens investigations into physicians or PAs who have had two or more patient deaths due to opioid poisoning within a 12-month period. NCMB wants to modify these criteria so that investigations would only be opened if the prescriber a) authorized 30+ tablets of an opioid to the decedent AND b) the opioid prescriptions were written within 60 days of the patient’s death.
Why does the Board want to make changes to the “patient deaths” criteria?
In the vast majority of cases where the prescriber authorized some type of controlled substance in the 12 months preceding the death, the prescribing did not contribute to the death. Adding filters to ensure that opioids were prescribed in close proximity to the death will ensure that cases are only opened on physicians or PAs who authorized recent opioid prescriptions.
How does NCMB want to change the “high-volume, high-dose” criteria?
Currently NCMB investigates the top ONE percent of licensees prescribing 100 morphine milligram equivalents (MMEs) per patient, per day. The Board also looks at prescribers who meet this criteria and also prescribe in combination with a benzodiazepine. The Board wants to begin opening cases into the top TWO percent of such prescribers.
Why does the Board want to expand the “high-volume, high-dose” criteria?
A majority of cases opened based on these criteria resulted in either private or public action, based on Board findings of substandard practice or other concerns regarding quality of care. The Board believes expanding these criteria to the top TWO percent of clinicians prescribing 100 MMEs per patient, per day, will likely identify additional prescribers who may not be practicing consistent with current accepted standards of care.
What other changes to the selection criteria is NCMB considering?
The Board is interested in creating a new set of selection criteria to identify prescribers whose practices display certain characteristics (See “Potential SOPI investigative criteria” below). The Board voted in January to test the proposed criteria before seeking rule changes to formally establish them.
How will these proposed changes affect the number of SOPI cases opened?
The Board expects to open fewer cases based on patient deaths than it did under existing criteria. It expects an increase in the number of cases related to the changes to the “high-volume, high dose” criteria.
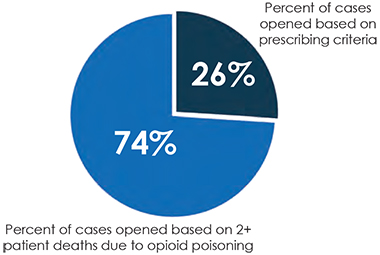
As the vast majority of SOPI cases to date have been opened based on the patient deaths criteria, the Board expects the net effect of the rule changes to be a smaller but more specific and sensitive report of licensees meeting any investigative criteria.
Cases Opened
As of January 2017 NCMB has completed 62 based on SOPI criteria. These cases have directly impacted .2% of the licensee population.
Current SOPI investigative criteria:
- • Top one percent prescribing 100 milligrams of morphine equivalents (MME) per patient per day.
• Top one percent prescribing 100 MMEs per patient per day in combi-nation with any benzodiazepine and within the top one percent of all con-trolled substance prescribers by vol-ume.
• Prescribers with two or more patient deaths within a 12–month period due to opioid poisoning.
Revised SOPI investigative criteria:
- • Top two percent prescribing 100 morphine milligram equivalents (MME) per patient per day.
• Top two percent prescribing 100 MMEs per patient per day in combination with any benzodiazepine and within the top one percent of all controlled substance prescribers by volume.
• Prescribers with two or more patient deaths within a 12–month period due to opioid poisoning AND authorized 30+ tablets of an opioid to the decedent AND scripts were written within 60 days of the patient’s death.
Potential SOPI investigative criteria *
NCMB would investigate prescribers who meet at least three of the following criteria:
- 1. At least 25 percent of the prescriber’s patients receiving opioids reside at least 100 miles from the prescriber’s practice location;
2. The prescriber has more than 30 patients receiving the same opioid and benzodiazepine combination;
3. A majority of the prescriber’s patients receiving opioids self-pay for the prescription;
4. Prescriber allows an early opioid prescription refill more than twice in the last 12 months;
5. More than 50% of the prescriber’s patients receive opioid doses of 100 MME or greater per day; or
6. The prescriber has more than ten patients who use three or more pharmacies within a year to obtain opioids.
* NCMB will study this criteria to determine its feasibility and value before pursuing rule changes.
The SOPI rule changes are available on the NCMB website in the Rule Change Tracker: www.ncmedboard.org/SOPIRules
Comments on this article:
Really a very fair plan that goes a long way toward weeding out the bad players while allowing normal practice to proceed.
I have one question, which may have been addressed elsewhere: How will the Board treat palliative care cases, where MEs and death rates are both likely to be high?
By Laura P Schulman, M.D. on Mar 02, 2017 at 1:48pm
A couple comments on the potential SOPI investigative criteria:
4. Prescriber allows an early opioid prescription refill more than twice in the last 12 months;
I presume this means early refill more than twice for a particular patient, not across the entire practice.
6. The prescriber has more than ten patients who use three or more pharmacies within a year to obtain opioids.
I would recommend this be a percentage of all patients on opiates in the practice rather than a specific number. A doctor who has 9 of a total of 10 of his opiate patients shopping pharmacies is more likely to have an issue (but be missed by the screen) than a pain specialist who has 10 out of 200 total opiate patients.
By Stephen Tuel on Mar 02, 2017 at 2:37pm
Thank you for your comment, Dr. Schulman. To date, none of the 62 cases opened based on the existing SOPI investigative criteria have involved prescribers who practice hospice or palliative medicine. To show up as a “hit” based on the patient deaths criteria, the patient deaths would have to be listed as opioid toxicity. For most patients who die under the care of a hospice or palliative provider, the cause of death is something else (e.g. cancer).
By Jean Fisher Brinkley on Mar 03, 2017 at 2:07pm
I am a hospice/palliative medicine provider and I can easily see that I would potentially meet 3 of 6 of the SOPI criteria. I work exclusively at a cancer center, practicing Palliative Med/Oncology, and many of my patients travel a great distance to see me, as well as their oncologist. I think it should be considered that physicians that exclusively practice HPM be exempt from the SOPI criteria. Many of my patients use different pharmacies for their long acting opiates, especially those from small rural areas, since their local pharmacies frequently don’t carry their medications. Early refills are not unusual when most of your patients have incurable malignancies and frequent pain crises.
By Beth Susi on Mar 03, 2017 at 3:12pm
All of the board actions are “after the fact” (or death) actions. Is there any consideration to requiring CME or training (especially to new graduates) as to safe prescribing practices for controlled substances or addiction or risk mitigation for prescribing ? It concerns me how easy DEA licenses are obtained without any concern for the prescribers ability to judge risk.
By John Rouchard on Mar 07, 2017 at 8:27am
